Case-files (DR)
List of case-files from seminars with DR
4. 58y man with sepsis
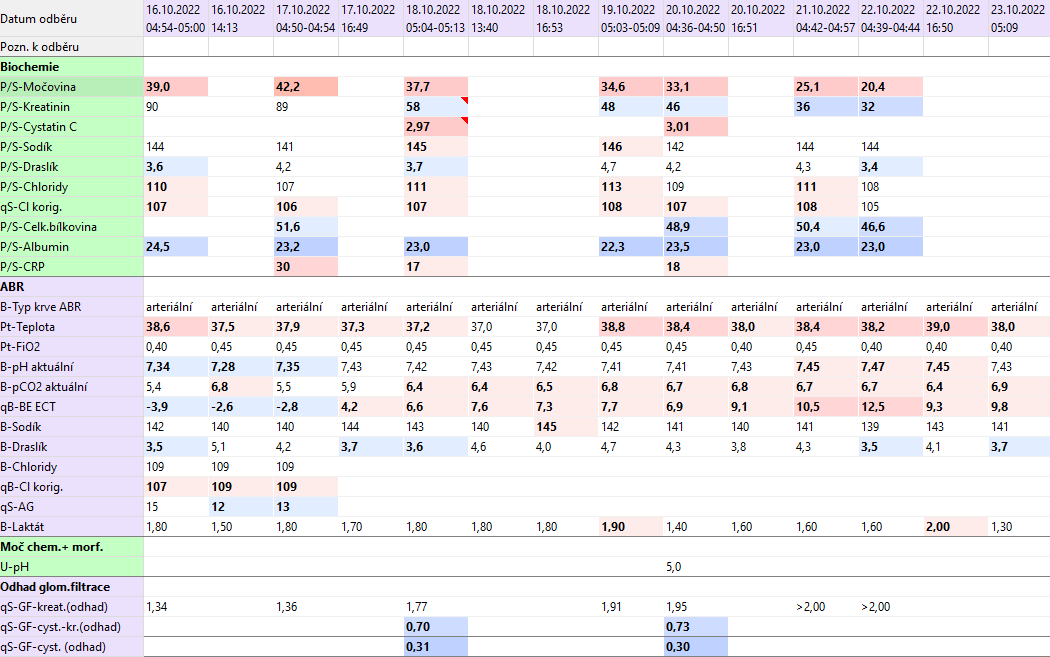
58-year-old patient, obese, chron. bronchitis, art. hypertension, manic-depressive psychosis according to documentation. In the past, after surgery for perforation of a duodenal ulcer with a complicated course, revision of the abdominal cavity for abscesses, closure of the abdominal wall with Prolen mesh. On 27.9. admitted in a severe condition, septic, with an incarcerated hernia in the scar (one of the hernias in the lower part of the laparotomy), hypotensive, anuric, shock condition. From the vital indication on 27.9.2022, multiple lysis of adhesions was performed, resection of the blood pressure for gangrene during incarceration in the hernia, toilet of the abdominal cavity, drainage. Postoperatively in the ICU II CHK at the UPV. Circulatory support, deterioration of liver and kidney parameters, progression of inflammation parameters gradually progress. On 29.9. a transverostomy was established after resection of a part of the transverse for ischemia. Postoperatively, a slight reduction in circulatory support, a slight improvement in organ dysfunction, but practically without interruption of the febrile continuum, the wound was anergic with no signs of healing. On 3.10., repeated deterioration of ventilation parameters (mainly oxygenation function), X-ray signs of congestion in the small circulation - aggressive ventilation support + dobutamine with a positive effect on ventilation, but fever persists, drains on the left side began to drain enteral contents (proven by application of methylene blue p.o.). Due to the enormous surgical risk and stabilization of the patient (improvement of laboratory parameters, reduction of circulatory support), despite the fever, the conservative procedure continued in agreement with the clinic management. Gradually discontinued support with Dobutamine. Subfebrile fever with febrile spikes persists. On 10.10. for enteral secretion through the wound and all drains indicated for rust on the OS due to vital indication. The source is point perforation of the jejunum, its resection was performed, a laparostomy was established. Postoperative recurrence of septic shock with high catecholamine support. After volumoterapy, circulatory support has been reduced. However, enteral waste from drains appears again. Repeated redressing of laparostomy. On 24.10., in case of a satisfactory finding, the abdominal cavity was closed with a composite mesh. Cushioning and weaning started. Currently without muscle strength. He opens his eyes to address him, tries to nod his head. On 1.11. re-development of subfebrile to febrile tips - signs of urinary infection - ATB was administered, PMK exchange. Nutrition for NGS with good tolerance, gradually discontinued PN. After damping, the manifestations of polyneuropathy in critically ill patients are clearly expressed - now there is already a hint of a handshake. CT scan was performed - brain without signs of haemorrhage or older ischemia, inflammatory infiltrations bilateral on the lungs, BP distension on the abdomen, but with a functional stoma. In the evening of 25.11. severe circulatory instability with stable sinus image, manifestations of sepsis, febrile.Circulatory support, volumotherapy is significantly increased - so far no effect. Severe acidosis in the laboratory. X-ray S+P performed - lungs unfolded without clear lesion. Change of ATB according to the last bacteriol. On 26.11. continued to subside and continued UPV, persistent ferbilia, the condition requires maximum doses of catecholamine support, marbling of the limbs and abdominal wall appears. Anuric. Drains from the abdominal cavity with persistent purulent secretion. Finding consistent with severe sepsis with source in the abdominal cavity. The patient is not tolerable to be transported to a CT scan, another surgical solution is technically impracticable. Ill in serious condition since the end of 9/2022, exhausted. On 26.11. at 9.45 a.m. Exitus letalis. A pathological-anatomical autopsy confirms the above diagnoses.
Questions
- What muscle mass do you expect the patient to have around 16.10.? What was it around 18.10.?
- Which laboratory markers will help you in estimating a patient's nutritional status?
- What effects may limit the use of cystatin C in this patient?